54year old female with CKD
A 54yr old female home maker resident of Nalgonda came to opd with chief complaints of breathless since 10days cough since 10days ,fever since 10days ,swelling in the legs and facial puffiness since 10days and vomiting since 7days
HOPI
patient was apparently asymptomatic 10days ago the she developed shortness of breath which was insidious in onset gradually progressive in nature and aggravating on walking and relived on sitting position grade 3 according to mmrc grading
No h/o orthopneia
No h/o paraoxysmal nocturnal dyspnea
Bilateral Pedal edema since 10days which was pitting type seen near the ankles insidious in onset and gradually progressive in nature
Facial puffiness since 10days started near orbits and gradually progressed to entire face
Cough since 10days insidious in onset, gradually progressive ,productive type ,white in color,in small quantity,non foul smelling,non blood stained,with no diurnal variation,with no aggravating and relieving factors
Fever since 10 days insidious onset ,gradually progressive,low grade,intermittent type,associ with chills ,rigors ,body pains with no diurnal variation,relieves temporarily with medication, no aggravating factors
Vomiting since 7 days non projectile type non blood stained,non foul smelling ,content is food,with 2-3 episodes per day but on Saturday she had 5 episodes of vomiting
Past history:
K/c/o Asthma since 20 years -patient is on Salbutamol
K/c/o hypertension since 10 years-patient is on medication atenolol
-she is having a history of fever 4years ago for which she went to hospital and doctor suspected of having kidney problem and gave sodium bicarbonate.
-No history of diabetes mellitus,tuberculosis,epilepsy
-No history of previous surgeries.
Personal history-
diet -mixed
Sleep-adequate
Appetite-reduced since 10 days
Bowel and bladder movements-regular
Addictions-none
Family history-no significant family history
General physical history:
Patient conscious coherent cooperative moderately built and nourished
No pallor,icterus, cyanosis,clubbing,lymphadenopathy,edema
Temperature :
Pulse Rate: 80 beats per minute
Respiratory rate: 18 times per minute
BP:
SpO2 : 87% at room temperature
GRBS- 95 mg / dl
Systemic examination
Respiratory
On inspection
Nose
No structural abnormalities found in nose
No obstruction in nose and nasal polyps are seen
Oral cavity
No oral lesions
No crooked teeth
Trachea
Appears to be central
Chest
Bilateral symmetrical
Elliptical in shape
Chest expansion is equal on both sides
No engorged veins are seen
PALPATION
No local rise in temperature and no tenderness
The position of trachea is confirmed by 3finger test
Apical impulse present
Chest expansion is equal on both sides
Anterior posterior diameter-17cm
Transverse diameters-28cm
Vocal fremitus
They are equal on both sides
Percussion Right Left
Supraclavicular | Resonant | Resonant |
Infraclavicular | Resonant | Resonant |
Axillary | Resonant | Resonant |
Infraaxillary | Resonant | Resonant |
Suprascapular | Resonant | Resonant |
Infra scapular | Resonant | Resonant |
Interscapular | Resonant | Resonant |
Mammary | Resonant | Resonant |
Auscultation
Right | Left |
Supraclavicular | Nvbs | Nvbs |
Infraclavicular | Nvbs | Nvbs |
Axillary | Nvbs | Nvbs |
Infraaxillary | Nvbs | Nvbs |
Suprascapular | Nvbs | Nvbs |
Infrascapular | Nvbs | Nvbs |
Interscapular | Nvbs | Nvbs |
Mammary | Nvbs | Nvbs |
Per abdomen examination:
On inspection
Shape of abdomen : scaphoid
Umbilicus : inverted
Movements of abdomen wall with respiration
No visible peristalsis, pulsations, sinuses, engorged veins, hernial sites
On palpation
No local rise of temperature
Inspectory findings are confirmed
Soft and non tender
No palpable mass
Liver and spleen not palpable
On percussion
Tympanic note heard
On auscultation
Bowel sounds heard
CVS examination:
S1 S2 heard
No murmurs heard
CNS examination :
No focal neurological deficits
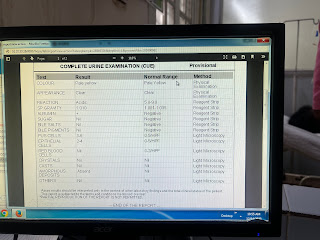
Investigations











Comments
Post a Comment